Introduction
Obsessive-Compulsive Disorder, commonly known as OCD, is a mental health condition that affects millions worldwide. It involves intrusive, unwanted thoughts (obsessions) and repetitive behaviors or mental acts (compulsions) that individuals feel driven to perform.
Understanding OCD accurately is crucial, as misconceptions can lead to stigma and prevent people from seeking help.
This blog post aims to provide clear, evidence-based answers to frequently asked questions about OCD. We will explore its definition, symptoms, causes, diagnosis, treatment options, and impact on daily life, drawing on the latest research and clinical insights.
Our goal is to offer a comprehensive resource for individuals with OCD, their families, and anyone seeking to learn more about this complex disorder.
Section 1: Understanding OCD Basics
What is OCD?
Obsessive-Compulsive Disorder (OCD) is characterized by uncontrollable, recurring thoughts, known as obsessions, and repetitive behaviors, known as compulsions, that a person feels compelled to repeat (NIMH).
These symptoms can significantly interfere with daily activities and cause considerable distress.
What is the full form of OCD?
The full form of OCD is obsessive-compulsive disorder.
What is the difference between OCD and OCPD?
While OCD and Obsessive-Compulsive Personality Disorder (OCPD) share similar names, they are distinct conditions.
OCD is a mental health disorder defined by the presence of obsessions and compulsions, often causing significant distress (American Psychiatric Organization). Individuals with OCD usually recognize their thoughts or behaviors as excessive or unreasonable.
In contrast, OCPD is a personality disorder characterized by a pervasive pattern of preoccupation with orderliness, perfectionism, and control (MSD Manual).
People with OCPD typically do not experience specific obsessions or compulsions in the same way as those with OCD. Their rigid traits are often seen as part of their personality (ego-syntonic), and they may not view their behavior as problematic (Cleveland Clinic)
Is OCD a type of anxiety disorder or depression?
Historically, OCD was classified as an anxiety disorder due to the significant anxiety associated with obsessions and compulsions.
However, in the latest diagnostic manuals like the DSM-5, OCD is now categorized under its own chapter, “Obsessive-Compulsive and Related Disorders.” This reflects a better understanding of its unique features.
While OCD is distinct from anxiety disorders and depression, it frequently co-occurs with them (Healthline). Many individuals with OCD also experience significant symptoms of anxiety or depression, which often require separate attention during treatment.
Is obsession a mental illness?
Experiencing occasional obsessive thoughts is common and not necessarily indicative of a mental illness.
However, when obsessions become persistent, intrusive, unwanted, and cause significant distress or impairment in daily functioning, they are a core symptom of obsessive-compulsive disorder (OCD), which is a recognized mental illness (Mayo Clinic).
Section 2: OCD Prevalence and Demographics
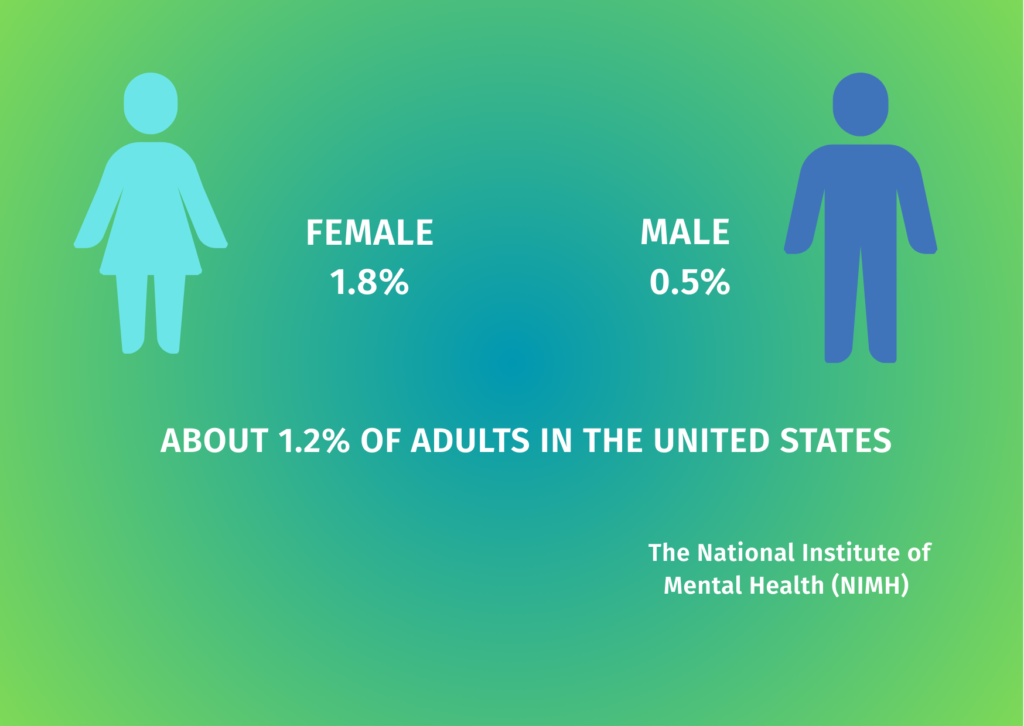
How common is OCD?
According to Medical News Today, approximately 1.2% of U.S. adults had OCD in the past year. The lifetime prevalence of OCD among U.S. adults is estimated at 2.3%. The Cleveland Clinic reports that OCD affects between 1.6% and 2.3% of the general U.S. population.
OCD is more common in females (1.8%) than in males (0.5%), according to NIMH statistics. The International OCD Foundation estimates that about 1 in 40 adults (2.5%) have OCD or will develop it at some point in their lives, which translates to approximately 8.2 million adults in the United States.
Who does OCD affect?
OCD affects people of all races, ethnicities, genders, and backgrounds (International OCD Foundation). While OCD can develop at any age, from preschool to adulthood, there are two common age ranges when OCD tends to first appear:
1. Between the ages of 7 and 12
2. During late adolescence and early adulthood (around age 20)
Research indicates that OCD symptoms can begin earlier in males than in females, with males often showing symptoms in childhood, while females more commonly develop symptoms in adolescence or early adulthood.
Who suffers from OCD the most?
While OCD can affect anyone, research suggests certain demographic patterns. As mentioned earlier, OCD is more prevalent in females than males in adulthood. However, childhood-onset OCD is more common in boys than girls.
The severity of OCD can vary widely among individuals. According to the National Institute of Mental Health, of those with OCD, 50.6% experienced severe disruptions in their daily lives, 34.8% experienced moderate disruptions, and 14.6% experienced mild disruptions.
Section 3: OCD Symptoms and Types
What are the symptoms of OCD?
OCD is characterized by two main components: obsessions and compulsions.
Obsessions are persistent, unwanted thoughts, urges, or images that are intrusive and cause anxiety or distress. These thoughts are not simply excessive worries about real-life problems.
The person experiencing them often tries to ignore or suppress these thoughts or neutralize them with another thought or action (a compulsion).
Compulsions are repetitive behaviors or mental acts that a person feels driven to perform in response to an obsession or according to rigid rules.
These behaviors or mental acts aim to reduce anxiety or prevent a feared event, but they are either not realistically connected to what they’re designed to neutralize or are clearly excessive.
For a diagnosis of OCD, these obsessions and compulsions must:
– Causes significant distress
– Be time-consuming (take more than 1 hour per day)
– Significantly interfere with the person’s normal routine, occupational functioning, or social activities and relationships
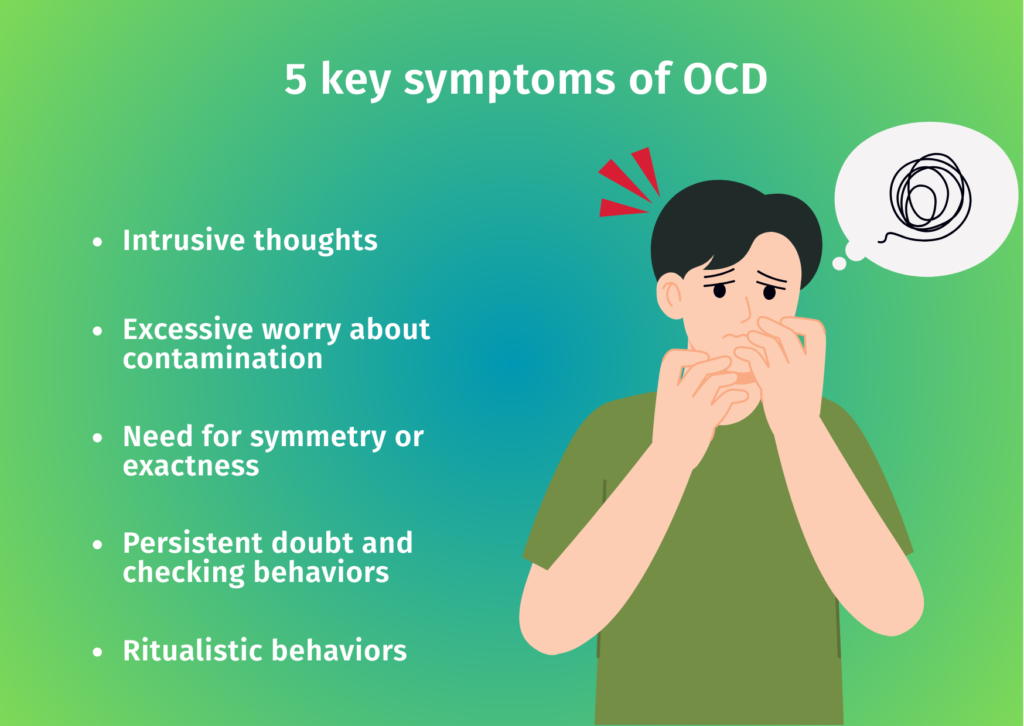
What are the 5 key symptoms of OCD?
Five key symptoms that characterize OCD include:
1. Intrusive thoughts: Unwanted, persistent thoughts, images, or urges that cause anxiety or distress
2. Excessive worry about contamination: Fear of germs, disease, or feeling “unclean”
3. Need for symmetry or exactness: Strong urges to arrange items in a specific way or perform actions in a precise manner
4. Persistent doubt and checking behaviors: Repeatedly checking things like locks, appliances, or seeking reassurance
5. Ritualistic behaviors: Performing specific actions in a particular order or a set number of times to reduce anxiety
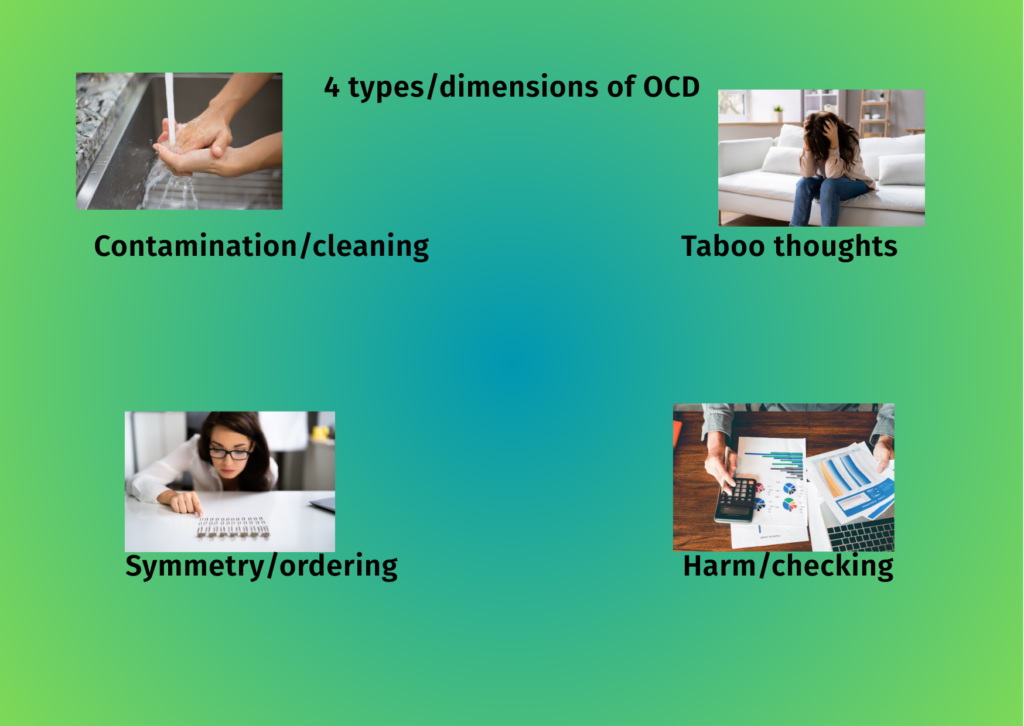
What are the 4 types/dimensions of OCD?
According to research published in Frontiers in Psychiatry, OCD symptoms typically cluster around four major dimensions:
1. Contamination/cleaning: Fear of germs, disease, or contamination leading to excessive washing and cleaning rituals
2. Symmetry/ordering: Need for things to be “just right,” symmetrical, or in perfect order
3. Taboo thoughts: Unwanted aggressive, sexual, or religious intrusive thoughts that cause significant distress
4. Harm/checking: Fear of harm coming to oneself or others, leading to extensive checking behaviors
It’s important to note that many individuals with OCD experience symptoms across multiple dimensions, and their symptoms may change over time.
What is OCD behavior?
OCD behavior refers to the compulsions or rituals that individuals perform in response to their obsessions. These behaviors are attempts to reduce anxiety or prevent a feared outcome, but they provide only temporary relief and ultimately reinforce the cycle of OCD.
Common OCD behaviors include:
– Excessive hand washing or showering
– Checking (doors, appliances, body parts) repeatedly
– Counting, tapping, or repeating certain words
– Arranging items in a specific order or symmetrical pattern
– Mental rituals like praying, counting, or “canceling” bad thoughts
– Seeking reassurance from others
– Avoiding situations that trigger obsessions
These behaviors are typically rigid, excessive, and time-consuming, significantly interfering with daily functioning.
Is overthinking OCD?
Overthinking alone is not OCD. Many people experience overthinking or rumination without having OCD. The key differences lie in the nature of the thoughts and the response to them.
In OCD, thoughts are typically:
– Intrusive and unwanted
– Distressing and anxiety-provoking
– Accompanied by compulsive behaviors or mental rituals to neutralize them
– Significantly interfering with daily functioning
General overthinking or worry tends to focus on real-life concerns (like work, relationships, or health), while OCD obsessions often involve themes that are unlikely or even impossible (like causing harm by thinking about it).
If overthinking is causing significant distress or impairment, it’s important to consult with a mental health professional for proper assessment and diagnosis.
OCD examples in daily life
OCD can manifest in various ways in everyday life. Here are some examples:
Contamination fears:
– Avoiding public restrooms or doorknobs
– Washing hands until they’re raw
– Using paper towels to touch doorknobs
– Excessive use of hand sanitizer
Checking behaviors:
– Repeatedly checking that the stove is off
– Checking multiple times that the doors are locked
– Returning home to verify that appliances are turned off
– Repeatedly checking emails for errors before sending
Symmetry and ordering:
– Needing items on a desk to be perfectly aligned
– Arranging books by size, color, or another specific order
– Feeling intense discomfort if items are not “just right”
– Rewriting notes until handwriting appears perfect
Intrusive thoughts:
– Unwanted violent or sexual thoughts
– Fear of blurting out inappropriate comments
– Intrusive religious or blasphemous thoughts
– Fear of accidentally harming someone
Mental rituals:
– Counting while performing tasks
– Silently repeating phrases or prayers
– “Canceling out” bad thoughts with good ones
– Mentally reviewing conversations or interactions
These examples illustrate how OCD can affect various aspects of daily life, from routine activities to social interactions and work performance.
Section 4: Causes and Development of OCD
What causes OCD?
OCD has no single, definitive cause. Research indicates it results from a complex interaction of multiple factors (International OCD Foundation, 2025):
Brain Differences: Studies show overactivity in specific brain regions, including the orbitofrontal cortex, anterior cingulate cortex, thalamus, and basal ganglia. These areas are involved in decision-making, error detection, and habit formation.
Neurotransmitters: While OCD isn’t solely caused by chemical imbalances, neurotransmitters like serotonin, dopamine, glutamate, and GABA appear to play important roles in the disorder.
Genetics: OCD has a significant genetic component. About 10-20% of children with a parent who has OCD will develop the condition themselves. A recent worldwide genetics study found OCD to be genetically related to other psychiatric disorders, including Tourette syndrome, anorexia, and anxiety disorders (UF Health).
Environmental Factors: Twin studies suggest that while genetics plays a stronger role than environment, non-shared environmental factors do contribute to OCD development.
PANDAS/PANS: In some children, OCD symptoms appear suddenly following infections, particularly strep throat. This condition, known as Pediatric Autoimmune Neuropsychiatric Disorders Associated with Streptococcal infections (PANDAS), represents a specific subtype of OCD with an autoimmune component.
Research from Nature confirms that OCD likely originates from a complex interaction of genetic and environmental risk factors, similar to other psychiatric disorders in its multifactorial origins.
What is the first stage of OCD?
OCD typically develops gradually, though some cases (particularly PANDAS) may have a sudden onset. The first stage often involves:
Early Warning Signs: Subtle changes in thinking patterns, including increased worry about certain themes (contamination, harm, symmetry, etc.) that go beyond normal concerns.
Initial Intrusive Thoughts: The appearance of unwanted, distressing thoughts, images, or urges that feel foreign to the individual’s character.
Beginning Anxiety Response: Heightened anxiety in response to these thoughts, with the person starting to believe the thoughts might be meaningful or dangerous.
Early Neutralizing Behaviors: Initial attempts to reduce anxiety through behaviors that will later develop into full compulsions. These might be simple at first, like brief checking or mental rituals.
At this early stage, symptoms may not yet meet the full criteria for OCD diagnosis, but early intervention can be crucial for preventing progression.
What are the four stages of OCD?
While OCD manifests differently in each individual, the disorder’s progression can often be conceptualized in four stages:
1. Obsession: Intrusive, unwanted thoughts, images, or urges enter the mind and cause significant distress.
2. Anxiety: These obsessions trigger intense anxiety, discomfort, or a sense that something terrible will happen if the person doesn’t respond in a specific way.
3. Compulsion: The person performs mental or physical rituals to reduce the anxiety caused by the obsession or to prevent the feared outcome.
4. Temporary Relief: Completing the compulsion provides short-term relief from anxiety, but this reinforces the cycle, making it more likely that the obsession will return and the compulsion will be repeated.
This cycle repeats continuously, often becoming more entrenched and time-consuming over time if left untreated.
What triggers OCD thoughts?
OCD triggers vary widely among individuals and may include:
Stress: Periods of high stress often exacerbate OCD symptoms or can trigger their initial onset.
Major Life Transitions: Changes such as starting school, beginning college, entering the workforce, marriage, or having children can trigger or worsen OCD.
Trauma: Traumatic experiences can sometimes trigger the development of OCD in genetically predisposed individuals.
Illness or Health Concerns: Personal illness or health scares, or those affecting loved ones, can trigger contamination or harm-related OCD.
Hormonal Changes: Some women experience new or worsened OCD symptoms during pregnancy, postpartum, or at other times of hormonal fluctuation.
Media Exposure: News stories about disasters, crimes, or diseases can trigger OCD thoughts in vulnerable individuals.
Environmental Cues: Specific situations, locations, or objects associated with previous obsessions can trigger OCD thoughts through conditioning.
Understanding personal triggers can be an important part of OCD management, though treatment typically focuses on changing responses to triggers rather than avoiding them entirely.
Section 5: Diagnosis and Assessment
How is OCD diagnosed?
OCD diagnosis involves a comprehensive assessment by qualified mental health professionals. According to the Mayo Clinic, diagnosis typically includes:
Psychological Evaluation: A detailed discussion about thoughts, feelings, symptoms, and behavior patterns to identify obsessions and compulsions that interfere with quality of life. With permission, this may include talking to family members or friends.
Physical Exam: This may be conducted to rule out other medical conditions that could cause similar symptoms and to check for any related complications.
Diagnostic Criteria: Clinicians use established criteria from diagnostic manuals like the DSM-5 to determine if symptoms meet the threshold for OCD diagnosis.
Differential Diagnosis: OCD symptoms can resemble those of other mental health disorders, including obsessive-compulsive personality disorder, anxiety disorders, depression, and schizophrenia. It’s also possible to have OCD alongside another mental health condition.
OCD test methods
Several validated assessment tools help clinicians diagnose and measure the severity of OCD (International OCD Foundation):
Diagnostic Interviews:
– Anxiety Disorders Interview Schedule for DSM-IV (ADIS)
– Structured Clinical Interview for DSM-IV (SCID)
Clinician-Administered Scales:
– Yale-Brown Obsessive-Compulsive Scale (Y-BOCS) is the most widely used severity rating scale for OCD
– Children’s Yale-Brown Obsessive-Compulsive Scale (CY-BOCS) is for pediatric assessment
Self-Report Measures:
– Florida Obsessive Compulsive Inventory (FOCI)
– Obsessive Compulsive Inventory-Revised (OCI-R)
– Dimensional Obsessive-Compulsive Scale (DOCS)
Parent/Family Assessment:
– Family Accommodation Scale (FAS) measures how family members accommodate OCD symptoms
– Child Obsessive Compulsive Impact Scale (COIS), assesses impact on child functioning
According to NOCD, specialists often use structured interviews like the DIAMOND (Diagnostic Interview for Anxiety, Mood, and OCD-Related Neuropsychiatric Disorders) to ensure diagnostic criteria are met.
Difference between OCD and anxiety
While OCD was previously classified as an anxiety disorder and shares some features with anxiety disorders, there are important distinctions:
Nature of Thoughts:
– OCD: Involves specific intrusive thoughts, images, or urges that are unwanted and distressing
– Anxiety: Typically involves excessive worry about real-life concerns
Behavioral Response:
– OCD: Features compulsive behaviors or mental rituals performed to reduce anxiety or prevent feared outcomes
– Anxiety: May involve avoidance but typically lacks the ritualistic behaviors characteristic of OCD
Thought-Action Fusion:
– OCD: Often involves magical thinking, where having a thought is equated with acting on it
– Anxiety: Usually maintains distinction between thoughts and actions
Treatment Response:
– OCD: Responds best to specific forms of CBT, particularly Exposure and Response Prevention (ERP)
– Anxiety: Responds to a broader range of CBT techniques
Both conditions involve fear and distress, can significantly impact daily functioning, and often respond to similar medications. They can also co-occur in the same person.
Is overthinking OCD or anxiety?
Overthinking alone is not sufficient to diagnose either OCD or an anxiety disorder, as it can be a feature of both conditions as well as other mental health issues or simply a personality trait.
In OCD, overthinking typically:
– Centers on specific intrusive thoughts or obsessions
– Leads to compulsive behaviors or mental rituals
– Involves thoughts that are ego-dystonic (foreign to one’s self-image)
– Often includes magical thinking or thought-action fusion
In anxiety disorders, overthinking typically:
– Focuses on realistic worries about future events
– Involves excessive concern about multiple life domains
– Lacks the specific ritualistic responses seen in OCD
– May be more generalized and less focused on specific themes
The key to distinguishing between normal overthinking, OCD, and anxiety disorders lies in the nature, intensity, and impact of the thoughts, as well as the behavioral responses they trigger. A proper diagnosis requires assessment by a qualified mental health professional.
Section 6: Treatment Approaches
How is OCD treated?
According to the Mayo Clinic and the International OCD Foundation, OCD is primarily treated through two evidence-based approaches:
Psychotherapy: Cognitive Behavioral Therapy (CBT), particularly a specialized form called Exposure and Response Prevention (ERP), is considered the gold standard psychological treatment for OCD.
ERP involves gradually exposing the person to situations that trigger their obsessions while helping them resist performing compulsions. This helps break the reinforcement cycle and teaches the brain that anxiety will decrease naturally without compulsions.
Medications: Certain psychiatric medications, particularly selective serotonin reuptake inhibitors (SSRIs), can help control OCD symptoms. FDA-approved medications for OCD include:
– Fluoxetine (Prozac) for adults and children 7 years and older
– Fluvoxamine (Luvox) for adults and children 8 years and older
– Paroxetine (Paxil) for adults only
– Sertraline (Zoloft) for adults and children 6 years and older
– Clomipramine (Anafranil) for adults and children 10 years and older
The International OCD Foundation notes that about 70% of people benefit from ERP and/or medication for their OCD. Often, a combination of both approaches yields the best results.
For treatment-resistant cases, additional options may include:
– Intensive outpatient and residential treatment programs
– Deep brain stimulation (DBS) for adults with severe, treatment-resistant OCD
– Transcranial magnetic stimulation (TMS)
– Group therapy, teletherapy, or Acceptance and Commitment Therapy
Can OCD be cured?
While there is currently no definitive “cure” for OCD in the sense of permanently eliminating the condition, effective treatments can significantly reduce symptoms and help individuals manage the disorder successfully. Many people achieve substantial improvement or remission with proper treatment.
As per the Swiss Medical Network, OCD treatment may not result in a cure, but can help bring symptoms under control so they don’t dominate daily life. Depending on the severity, some individuals may need long-term, ongoing, or more intensive treatment to maintain their progress.
It’s important to understand that even after successful treatment, some individuals may experience periodic flare-ups of symptoms, particularly during times of stress.
However, having learned effective management strategies, they can often address these episodes more effectively than before treatment.
Can OCD go away?
Research on the long-term outcomes of OCD shows varied results. According to a 40-year follow-up study published in JAMA Psychiatry, improvement was observed in 83% of patients, including complete recovery in 20% and recovery with subclinical symptoms in 28%.
For some individuals, especially those with milder symptoms who receive prompt and appropriate treatment, OCD symptoms may diminish significantly or even appear to “go away.” However, for many others, OCD is a chronic condition that requires ongoing management.
Factors that may influence whether OCD symptoms remit include:
– Age of onset (childhood-onset OCD sometimes remits in adulthood)
– Severity of symptoms
– Presence of comorbid conditions
– Access to effective treatment
– Family history
– Stress management skills
Can you recover from OCD?
Recovery from OCD is possible and is increasingly recognized as a realistic goal. As per the International Journal of Neuropsychopharmacology, despite OCD being considered a persistent and disabling disorder, longitudinal studies report symptomatic remission rates ranging from 32% to 70%.
Recovery may look different for different people:
– Some achieve complete remission of symptoms
– Others experience a significant reduction in symptoms to a manageable level
– Many learn to function well despite having some residual symptoms
A meta-analysis of long-term studies found that more than half of patients achieved remission (defined as a Y-BOCS rating <16) over 5 years of follow-up. Remission rates in children and adolescents tend to be higher than in adults.
How to defeat OCD?
While “defeating” OCD completely may not be possible for everyone, these evidence-based strategies can help manage and overcome OCD symptoms:
Seek professional help: Work with qualified mental health professionals who specialize in OCD treatment.
Commit to ERP therapy: Exposure and Response Prevention is challenging but highly effective. It requires facing fears while resisting compulsions.
Consider medication: For many, medication can reduce symptom severity enough to make therapy more effective.
Practice mindfulness: Learning to observe thoughts without judgment can help reduce their power.
Read also: Life Awakening: Mindful Living Journey
Build knowledge: Understanding OCD mechanisms can help recognize and challenge OCD patterns.
Develop a relapse prevention plan: Identify early warning signs and have strategies ready if symptoms intensify.
Join support groups: Connecting with others who understand OCD can provide encouragement and practical tips.
Reduce accommodation: Work with family members to reduce enabling of OCD behaviors.
Manage stress: Since stress often exacerbates symptoms, stress management techniques can be helpful.
Be patient and persistent: Recovery is usually gradual, with ups and downs along the way.
How do I silence my OCD?
“Silencing” OCD completely is rarely possible, and attempts to suppress thoughts often backfire, making them more persistent. Instead, experts recommend:
Change your relationship with thoughts: Rather than trying to silence obsessions, learn to relate to them differently. Mindfulness techniques teach observing thoughts without engaging with them.
Practice acceptance: Accepting that intrusive thoughts will occur, without fighting them, paradoxically reduces their power.
Use ERP techniques: Exposure therapy helps you learn that anxiety will naturally decrease even without performing compulsions.
Implement the “delay” strategy: When urges arise, practice delaying your response, gradually increasing the delay time.
Refocus attention: When obsessions arise, gently shift focus to a valued activity rather than trying to force thoughts away.
Reduce rumination: Limit time spent analyzing thoughts or seeking certainty.
Use cognitive restructuring: Challenge cognitive distortions that fuel OCD, such as overestimation of threat.
The goal is not to eliminate thoughts entirely but to reduce their impact and your response to them.
Read Also: How to Stop Negative Thoughts
How to stop OCD false memories?
OCD-related false memories or memory doubts are challenging symptoms that can cause significant distress. Strategies to address them include:
Understand the mechanism: OCD can create doubt about memories or generate “false memories” through repeated questioning and checking.
Resist verification: Avoid checking, seeking reassurance, or mentally reviewing memories, as these reinforce the cycle.
Practice uncertainty tolerance: Learn to sit with the discomfort of not knowing with 100% certainty.
Use ERP specifically for memory doubts: Work with a therapist to develop exposures that target memory-related obsessions.
Challenge the importance of certainty: Question whether absolute certainty about a memory is necessary or possible.
Mindfulness for rumination: Use mindfulness techniques to reduce rumination about past events.
Medication: Some individuals find that appropriate medication reduces the intensity of memory-related obsessions.
A qualified OCD specialist can help develop a tailored approach for addressing false memory OCD.
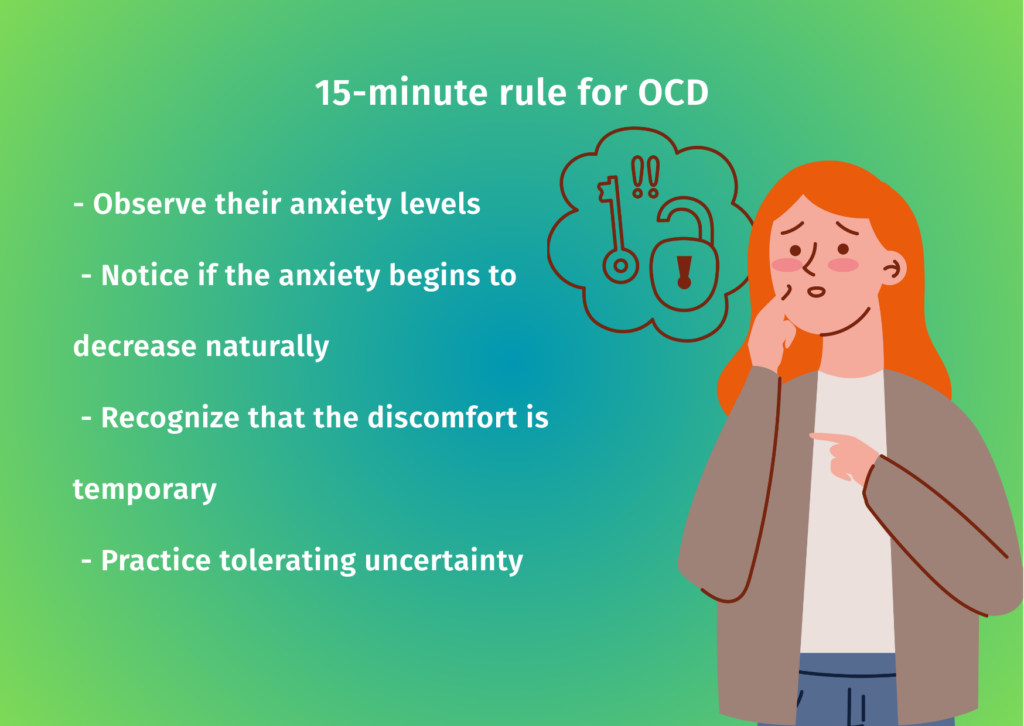
What is the 15-minute rule for OCD?
The 15-minute rule is a behavioral technique used in OCD treatment where patients agree to delay performing compulsions for at least 15 minutes when the urge arises. During this delay period, patients are encouraged to:
– Observe their anxiety levels
– Notice if the anxiety begins to decrease naturally
– Recognize that the discomfort is temporary
– Practice tolerating uncertainty
This technique helps break the immediate connection between obsessions and compulsions, demonstrating that anxiety will eventually decrease without performing rituals. As tolerance builds, the delay period can be gradually extended.
The 15-minute rule is often incorporated into Exposure and Response Prevention (ERP) therapy and helps individuals develop greater control over their responses to obsessive thoughts. It’s typically implemented under the guidance of a trained therapist as part of a comprehensive treatment plan.
Section 7: Living with OCD
How does OCD affect life?
OCD can significantly impact multiple areas of daily functioning. According to a study, people with OCD spend approximately 5.9 hours daily in obsessive thinking and 4.6 hours in compulsive acts, highlighting the time-consuming nature of the disorder.
Work Impact:
– Lost productivity due to time spent on rituals
– Difficulty meeting deadlines or completing tasks
– Challenges with concentration and focus
– Social isolation from colleagues
– Mental and physical exhaustion
– Excessive checking or perfectionism affecting performance
– Difficulty transitioning between tasks
Social Impact:
– Limited social connections due to avoidance behaviors
– Relationship strain from accommodation requests
– Difficulty maintaining natural conversations
– Canceled plans due to symptom flare-ups
– Embarrassment or shame about symptoms
– Misunderstandings from others about the nature of OCD
Family Life:
– Family members may become involved in rituals by providing reassurance
– Household routines may revolve around accommodating symptoms
– Increased tension and conflict about OCD behaviors
– Financial strain from treatment costs or reduced work capacity
– Emotional burden on family members
Educational Impact:
– Academic performance was affected despite intelligence and capability
– Perfectionism leading to incomplete assignments
– Difficulty with timed tests or exams
– Challenges with concentration in classroom settings
– Social isolation from peers
Physical Health:
– Sleep disruption from nighttime rituals or obsessions
– Physical injuries from excessive washing or checking
– Nutritional issues if food-related obsessions are present
– Exhaustion from the constant mental and physical demands of OCD
Despite these challenges, with proper treatment and support, many individuals with OCD lead fulfilling, productive lives while managing their symptoms effectively.
What should you avoid with OCD?
When managing OCD, certain approaches can be counterproductive:
Avoid accommodation: Family members providing reassurance or participating in rituals may temporarily reduce anxiety, but reinforce OCD patterns long-term.
Avoid thought suppression: Trying to force unwanted thoughts away often increases their frequency and intensity.
Avoid avoidance: Steering clear of triggers may provide short-term relief, but it strengthens OCD’s grip over time.
Avoid seeking certainty: Quests for absolute certainty fuel the OCD cycle; learning to tolerate uncertainty is essential.
Avoid self-criticism: Harsh self-judgment about having OCD symptoms can worsen anxiety and depression.
For those seeking to understand these emotional challenges more deeply and explore pathways to healing, Shining a Light on Depression: Finding Hope. The article underscores the importance of self-awareness, connection, and reclaiming agency over our mental well-being
Avoid comparing recovery: Each person’s OCD and recovery journey is unique; comparing to others can be discouraging.
Avoid all-or-nothing thinking: Recovery typically involves gradual improvement with occasional setbacks, not immediate perfection.
Avoid delaying treatment: Earlier intervention generally leads to better outcomes.
Avoid alcohol or substances: These may temporarily reduce anxiety but can interfere with treatment and worsen symptoms long-term.
Avoid isolation: While sometimes tempting, isolation often intensifies symptoms and prevents learning that fears are excessive.
Can OCD cause anger problems?
Yes, OCD can be associated with anger and irritability through several mechanisms:
Frustration: The constant battle with intrusive thoughts and compulsive urges can lead to significant frustration.
Interruption: When OCD rituals are interrupted or prevented, intense anger may result.
Perfectionism: When high standards can’t be met, anger directed at self or others may occur.
Exhaustion: The mental and physical toll of OCD can deplete emotional resources, lowering the threshold for irritability.
Family conflicts: Disagreements about accommodation or understanding of symptoms can trigger anger.
Comorbidity: OCD often co-occurs with other conditions that may include irritability as a symptom.
Medication side effects: Some medications used to treat OCD may have irritability as a side effect.
Treatment approaches that address anger in OCD include:
– Cognitive restructuring to identify and challenge anger-triggering thoughts
– Mindfulness techniques to recognize anger cues earlier
– Stress management and relaxation strategies
– Family therapy to improve communication and reduce conflict
– Addressing comorbid conditions that may contribute to anger
Does OCD affect memory?
Research suggests that OCD can impact memory functioning in several ways:
Memory confidence: People with OCD often have significantly reduced confidence in their memories, particularly for actions related to their obsessions (like checking if doors are locked).
Memory checking: Repeated checking paradoxically decreases memory certainty rather than increasing it.
Working memory: Some studies indicate that OCD may be associated with deficits in working memory, particularly when information is presented visually.
Memory biases: Individuals with OCD may have enhanced memory for threat-related information but impaired memory for positive or neutral information.
False memories: The doubt and uncertainty characteristic of OCD can sometimes lead to the creation of false memories or intense doubt about actual memories.
Cognitive load: The mental effort expended on obsessions and compulsions can reduce cognitive resources available for memory encoding and retrieval.
These memory effects are typically most pronounced for OCD-relevant situations rather than representing a general memory impairment. Effective OCD treatment often improves memory confidence and functioning.
How does OCD affect studying?
OCD can significantly impact academic performance and studying in several ways:
Perfectionism: Students with perfectionism-related OCD may spend excessive time on assignments, trying to make them “just right,” or avoid starting work altogether due to fear of imperfection.
Time management challenges: Compulsions can consume hours each day, leaving insufficient time for studying or completing assignments.
Concentration difficulties: Intrusive thoughts and mental compulsions can make it difficult to focus on learning materials.
Reading rituals: Some students develop rituals around reading, such as needing to read sentences or paragraphs multiple times until it “feels right.”
Writing challenges: Writing assignments may be particularly difficult due to concerns about word choice, sentence structure, or content.
Test anxiety: OCD can exacerbate test anxiety, with intrusive thoughts about failing or making mistakes interfering with performance.
Avoidance: Students may avoid certain classes, subjects, or educational settings that trigger OCD symptoms.
Classroom disruptions: The need to perform rituals may disrupt classroom participation or lead to frequent absences.
Strategies that can help include:
– Working with school counselors or disability services for accommodations
– Breaking assignments into smaller, manageable parts
– Setting time limits for tasks to prevent perfectionism
– Using external structures like timers or study buddies
– Applying ERP principles to academic situations
– Medication to reduce symptom intensity during critical academic periods
Which food is good for OCD?
While no specific diet has been proven to cure OCD, nutrition can play a supportive role in overall mental health and symptom management:
Omega-3 fatty acids: Found in fatty fish, flaxseeds, and walnuts, these may help reduce inflammation and support brain health.
Complex carbohydrates: Foods like whole grains, legumes, and vegetables help maintain stable blood sugar levels, which can reduce anxiety.
Antioxidant-rich foods: Colorful fruits and vegetables help combat oxidative stress, which may be elevated in some anxiety disorders.
Fermented foods: Yogurt, kefir, and other fermented foods support gut health, which is increasingly linked to mental health through the gut-brain axis.
Magnesium-rich foods: Leafy greens, nuts, and seeds may help with stress reduction and sleep quality.
Zinc-containing foods: Oysters, beef, pumpkin seeds, and lentils provide zinc, which plays a role in neurotransmitter function.
Vitamin D sources: Fatty fish, egg yolks, and fortified foods provide vitamin D, which may have mood-regulating effects.
Foods to consider limiting include:
– Caffeine, which can increase anxiety and interfere with sleep
– Alcohol, which may temporarily reduce anxiety but can worsen symptoms long-term
– Highly processed foods with artificial additives
– Foods that trigger individual sensitivities
It’s important to note that dietary changes should complement, not replace, evidence-based treatments like ERP and medication.
Can a person with OCD be normal?
The concept of “normal” is subjective and varies widely. People with OCD can absolutely lead fulfilling, productive, and meaningful lives that would be considered “normal” by most standards. Many successful professionals, artists, parents, and community members have OCD.
With effective treatment, many individuals with OCD experience significant symptom reduction and improved functioning. Even those with more persistent symptoms can develop strategies to manage them while pursuing their goals and maintaining relationships.
It’s important to recognize that OCD exists on a spectrum of severity. Some people have milder symptoms that respond well to treatment, while others may have more severe or treatment-resistant forms that require ongoing management.
Rather than focusing on “normality,” a more helpful framework might be considering quality of life, functioning in valued life domains, and personal satisfaction. Many people with OCD achieve high levels of all these measures with proper treatment and support.
Can people with OCD ever be happy?
Yes, people with OCD can absolutely experience happiness and lead fulfilling lives. While OCD can be challenging and distressing, several factors contribute to happiness potential:
Effective treatment: With proper treatment, many individuals experience significant symptom reduction, creating more space for positive experiences.
Acceptance: Learning to accept the presence of OCD while not letting it dictate life choices can be liberating.
Meaning and purpose: Engaging in meaningful activities aligned with personal values contributes to well-being regardless of OCD status.
Supportive relationships: Strong social connections provide joy and buffer against OCD-related distress.
Resilience development: Managing OCD often builds psychological resilience that enhances coping with life’s challenges.
Mindfulness skills: Techniques learned in OCD treatment can increase present-moment awareness and appreciation.
Reduced self-stigma: Separating identity from OCD symptoms (“I have OCD” rather than “I am OCD”) supports self-compassion.
Research on recovery in OCD increasingly recognizes that happiness and satisfaction are achievable goals, even if some symptoms persist. Many individuals report that OCD has contributed to personal growth, increased empathy, and a deeper appreciation for mental health.
Can an OCD person live alone?
Yes, many people with OCD can and do live independently. The ability to live alone depends on several factors:
Symptom severity: Individuals with milder symptoms or well-managed OCD often function independently without significant difficulty.
Treatment status: Those actively engaged in effective treatment typically develop skills that support independent living.
Functional impairment: Some severe OCD symptoms might temporarily interfere with self-care or home management, potentially requiring support.
Comorbid conditions: The presence of other mental health conditions alongside OCD may impact independent living capacity.
Support network: Even when living alone, having accessible support from friends, family, or treatment providers is beneficial.
Coping skills: Strong coping strategies and stress management techniques enhance successful independent living.
For some individuals with very severe OCD, temporary supported living arrangements during acute episodes might be helpful. However, with proper treatment, many return to independent living.
Living alone can sometimes present unique challenges for people with OCD (such as having no one to provide reality checks for OCD thoughts), but it can also reduce accommodation from well-meaning but counterproductive family members.
Can I marry an OCD person?
Yes, people with OCD can and do have successful, fulfilling marriages and relationships. Important considerations include:
Education about OCD: Understanding OCD as a medical condition rather than a personality flaw or choice is crucial for both partners.
Communication: Open, honest communication about symptoms, triggers, and needs helps prevent misunderstandings.
Avoiding accommodation: Learning how to support without enabling OCD behaviors is important for relationship health.
Boundary setting: Establishing healthy boundaries around how OCD affects shared activities and spaces.
Separate identities: Recognizing that the person is not defined by their OCD and nurturing non-OCD aspects of the relationship.
Treatment involvement: Partners can play a supportive role in treatment while avoiding becoming a therapist.
Self-care: Partners need their own support systems and self-care practices.
Shared decision-making: Making collaborative decisions about managing OCD’s impact on family life.
Many couples report that navigating OCD together has strengthened their relationship through increased communication, empathy, and problem-solving skills. With proper treatment and mutual understanding, OCD need not prevent a loving, lasting marriage.
Section 8: Prevention and Prognosis
Can I prevent OCD?
Currently, there is no known way to definitively prevent OCD from developing. However, several strategies may help reduce risk or minimize severity:
Early intervention: Recognizing and treating early signs of OCD can prevent symptoms from becoming more severe and entrenched.
Stress management: Since stress can trigger or exacerbate OCD symptoms, developing healthy stress management techniques may be protective.
Parenting approaches: For children at higher risk (such as those with family members with OCD), avoiding excessive accommodation of anxiety and encouraging healthy risk-taking may be beneficial.
PANDAS/PANS prevention: Prompt treatment of streptococcal infections may help prevent the development of PANDAS, a subtype of childhood OCD.
Healthy lifestyle: Regular exercise, adequate sleep, and balanced nutrition support overall mental health and resilience.
Seeking help for trauma: Addressing traumatic experiences with professional support may reduce the risk of developing various mental health conditions, including OCD.
Reducing family accommodation: For families with OCD members, learning not to participate in or facilitate rituals may help prevent symptoms from worsening.
While these approaches may be helpful, it’s important to note that OCD has strong genetic and neurobiological components that cannot always be prevented through behavioral strategies alone.
What is the prognosis of OCD?
The prognosis for OCD varies considerably among individuals, but research provides several insights:
Treatment response: About 70% of people with OCD show significant improvement with evidence-based treatments like ERP and/or medication (International OCD Foundation, 2025).
Remission rates: Longitudinal studies report symptomatic remission rates ranging from 32% to 70% (PMC ). A 40-year follow-up study found improvement in 83% of patients, including complete recovery in 20% and recovery with subclinical symptoms in 28% (JAMA Psychiatry).
Long-term outcomes: A meta-analysis of long-term studies found that more than half of patients achieved remission (YBOCS rating <16) over 5 years of follow-up (PMC, 2018).
Childhood vs. adult onset: Remission rates in children and adolescents tend to be higher than in adults, suggesting a better prognosis for early-onset cases that receive prompt treatment.
Factors affecting prognosis:
– Earlier age of onset (excluding very early childhood onset)
– Shorter duration of symptoms before treatment
– Good insight into the irrational nature of obsessions
– Absence of comorbid conditions
– Strong social support
– Access to expert treatment
– Adherence to treatment recommendations
While OCD was once considered an invariably chronic condition, contemporary research suggests that recovery is a realistic goal for many individuals, especially with appropriate treatment.
Even for those with more persistent symptoms, significant improvement in quality of life and functioning is often achievable.
Conclusion
Obsessive-Compulsive Disorder is a complex condition that affects millions of people worldwide. Through this comprehensive FAQ guide, we’ve explored the many facets of OCD from its definition and symptoms to its causes, diagnosis, treatment options, and impact on daily life.
If you or someone you know is experiencing symptoms of OCD, it’s important to seek help from qualified mental health professionals who specialize in OCD treatment. With proper diagnosis and treatment, the outlook for people with OCD is more promising than ever before.
For additional support and resources, consider connecting with organizations like the International OCD Foundation, which provides education, resources, and support for individuals affected by OCD and related disorders.
Remember that OCD is a medical condition, not a personal failing or character flaw. With understanding, treatment, and support, people with OCD can lead fulfilling, productive, and joyful lives.
Disclaimer: This article is for informational purposes only and is not a substitute for professional medical or mental health advice. Always seek the guidance of a qualified health professional with any questions you may have regarding your health or a medical condition.